Developing a Mobile-Based Exercise Program to Reduce Fear of Falling
ⓒ 2024 Korean Academic Society of Rehabilitation Nursing http://www.kasren.or.kr
Abstract
This study aimed to develop a mobile-based exercise program using cognitive behavioral principles to reduce fear of falling (FOF) in older adults after hip fracture surgery.
We developed a mobile application in the analysis-design-development-implementation-evaluation order. The mobile-based exercise application comprised multimedia education using the cognitive behavioral principles, resistance training video, coping cards, and positive feedback, which was developed from March to August 2023.
Four experts provided feedback on the content and usability. All experts perceived that the mobile application was useful and applicable in reducing FOF. There were also some comments for further improvement, and the mobile application was revised according to the experts’ comments. In addition, ten older adults who had undergone hip fracture surgery evaluated the application’s usability and satisfaction. Most older adults rated the application as reliable, easy to understand, helpful in reducing FOF, with a readable font and size, and satisfactory in its design.
This program will likely contribute to FOF reduction in older adults after hip fracture surgery by replacing negative emotions with positive ones and improving physical strength and balance.
Keywords:
Fear, Frail elderly, Hip fractures, Mobile applications, ExerciseINTRODUCTION
Fear of falling (FOF) is a highly prevalent symptom occurring in approximately 49% of older adults at 4~6 months (Jaatinen et al., 2022) and 47.5% at 6~12 months (Lee et al., 2023) after hip fracture surgery. FOF significantly impairs physical function, increases the risk of subsequent falls, and is associated with elevated short-term mortality (Ko et al., 2019; Mackay et al., 2021). FOF is a concern in the conduct of various activities of daily living (Delbaere et al., 2010). Excessive FOF, which leads to avoidance of daily activities, can have profound adverse effects on the health of older adults (Whipple et al., 2018). Effective methods for reducing FOF are limited for older adults after hip fracture surgery despite its high prevalence and significant impact on older adults’ health outcomes.
Exercise interventions have revealed a small to moderate reduction in FOF immediately after interventions. However, empirical evidence determining whether exercise interventions have a sustained effect on reducing FOF beyond the intervention period is insufficient (Kendrick et al., 2014). Exercise interventions are also costly and are considered barriers to a wide implementation in healthcare settings (Cody et al., 2020). Most importantly, after hip fracture surgery, older adults present with physical frailty secondary to underlying diseases and poor mobility (Ko et al., 2021); thus, visiting healthcare institutions poses as a challenge. Thus, exercise programs that allow easy access are necessary to ensure long-term adherence.
To address these challenges, this study developed an exercise program to reduce FOF, facilitated by mobile-based cognitive behavioral principles. This program design was informed by a scoping review (Whipple et al., 2018) highlighting the effectiveness of multi-component interventions incorporating exercise and cognitive behavioral therapy (CBT). The mobile-based cognitive behavioral principles were achieved via educational modules through the identification of unhelpful thoughts and fearful feelings that strengthen activity avoidance. CBT-based interventions have been commonly used and revealed to be effective in the management of FOF (Chua et al., 2019; Liu et al., 2018; Whipple et al., 2018). With CBT, motivation strategies to change the inappropriate perception toward an event allow older adults to control their emotions and maladaptive behaviors (Chua et al., 2019; Liu et al., 2018). Therefore, a sense of control of their FOF can be achieved by older adults, resulting in long-term adherence to physical activities.
Planned, structured, purposive, and repetitive exercise may reduce FOF (Kendrick et al., 2014). In reducing FOF, the effective types of exercise highlighted on enhancing strength, balance, agility, and flexibility (Whipple et al., 2018). This is because a decrease in muscle mass, strength, and power lead to an increase in FOF (Trombetti et al., 2016). This study employed resistance training that has been proven to improve muscle mass, strength, and functional capacity for the frail elderly (Lopez et al., 2018) to perform just after discharge. A well-designed resistance training program enhances aversion to catastrophic events including falls and improves the psychosocial well-being of older adults (Fragala et al., 2019).
A mobile application was adopted as a platform to employ the exercise program based on cognitive behavioral principles to older adults. Smartphones, with the advancement of mobile technology, can be used beyond time and place as part of healthcare education (Wang et al., 2018). The use of electronic technology considerably increased among older adults during the coronavirus pandemic. However, a remarkable number of older adults with difficulties in retrieval of health information from smartphones remain (Liu et al., 2022). The nursing field is therefore challenged to develop electronic technology-based interventions to provide better and reliable health care (Cody et al., 2020). The coronavirus pandemic greatly contributed to the development of online healthcare, and in the post-pandemic era, more and more older adults are likely to access these electronic devices (Liu et al., 2022).
To the best of knowledge, studies investigating exercise programs based on cognitive behavioral principles to reduce FOF in a mobile application remain limited. Furthermore, online interventions that lack ongoing interaction have demonstrated only modest effectiveness in managing FOF (Whipple et al., 2018). In this study, a mobile-based exercise program was developed to address these limitations. This program includes cognitive behavioral educational materials and resistance trainings, with participants receiving interactive support from a nurse practitioner via telephone. This study elucidates on the development and evaluation of the mobile-based exercise program. The study findings will provide evidence in helping older adults in using the exercise program via the mobile application to reduce FOF.
METHODS
We developed a mobile application in the analysis-design-development-implementation-evaluation order (Seels & Richey, 1994). The implementation and evaluation will be presented in the results.
1. Analysis
FOF is significantly higher among older adults following hip fracture surgery compared to both health older adults (Lee et al., 2023) and frail community-dwelling older adults (Martinez-Arnau et al., 2021). This increased FOF is attributed to the fact that hip fractures in older adults predominantly result from simple falls (Ko et al., 2021; Lee et al., 2023). Furthermore, many older adults fail to recover preoperative activities of daily living within one year post-surgery, despite their desire to resume simple daily activities (Ko et al., 2021). Addressing FOF is critical, as it has been identified as the most significant factor contributing to functional decline after hip fracture surgery (Ko et al., 2019).
To address FOF, cognitive behavioral principles were employed in designing an effective exercise program. To develop cognitive behavioral education, Beck’s book (Beck, 2017), the ABC theory which is one of the essential concepts in CBT (Lam & Gale, 2000), and world guidelines for falls prevention (Montero-Odasso et al., 2022) were used. The cognitive behavioral education component emphasized the role of unhelpful and negative thought patterns in shaping emotions and behaviors, as well as strategies for cognitive restructuring.
To analyze the characteristics and effects of the exercise interventions, a systematic review (Lopez et al., 2018) of 16 intervention studies related to resistance training was considered. To devise the content of the exercise program, the scientific and clinical application of elastic resistance (Rovny, 2004), previous studies of exercise programs using Thera-bands (Kim & Nam, 2011; Kim et al., 2007) were reviewed. These studies support the efficacy of elastic resistance exercise in improving muscle strength and flexibility, while also highlighting their safety, adaptability, low-risk profile, and cost-effectiveness.
2. Design
Literature reviews and periodic meetings with authors were used to create the contents of the mobile application. The mobile-based exercise application included two key components: multimedia cognitive behavioral education and coping cards for the cognitive behavioral intervention, and resistance training videos with positive feedback for the exercise intervention.
Multimedia cognitive behavioral education and coping cards. Multimedia cognitive behavioral education comprised of four parts: definition and consequences of FOF, and the relationship with cognition, emotion, and behavior in the first part; two cases of cognitive behavioral education in older adults with FOF in the second and fourth parts; and strategies for reducing FOF and creating environments to prevent falls in the third part. The cognitive behavioral education contents were reviewed by a psychologist to ensure aptness and comprehension for older adults.
We considered coping cards as a message of alternative thinking (Lam & Gale, 2000) to change unhelpful beliefs into helpful ones, in relation to a negative event causing FOF. The coping cards emphasized identifying, challenging, and restructuring maladaptive thoughts. It may mainly comprise of affirmations, reminders, action steps, and evidence-based reframes after interacting with older adults (Beck, 2017). The coping cards will be created after interacting with a psychiatric nurse practitioner via telephone intervention. During these 10-minute sessions, conducted biweekly, the nurse practitioner will identify participants’ negative thoughts or triggers related to daily activities and assist in reframing these into balanced statements.
Resistance training video and positive feedback. A senior physical education professor designed the contents of the resistance training according to the instructions for previous studies (Kim & Nam, 2011; Kim et al., 2007; Rovny, 2004). It comprised of nine exercises, including arm flexion and extension with shoulder extension, arm pull, torso rotation, ankle flexion, ankle lift, thigh strengthening, leg opening and closing, hip joint exercise, and thigh pull using a Thera-band. Each resistance training included one set of eight repetitions, and a yellow Thera-Band, representing the lowest intensity, was used initially twice daily. Exercise frequency and the Thera-band load will gradually increase after interacting with participants. The videos were created using a camera and were uploaded to a private YouTube account to ascertain that only the invited participants could view the videos.
The provision of positive feedback enables participants to enhance self-efficacy of exercise (Chua et al., 2019; Ha & Cho, 2021). A sunflower image is projected on the screen whenever participants achieve their daily exercise goals, determined by the time spent viewing the resistance training videos.
3. Development
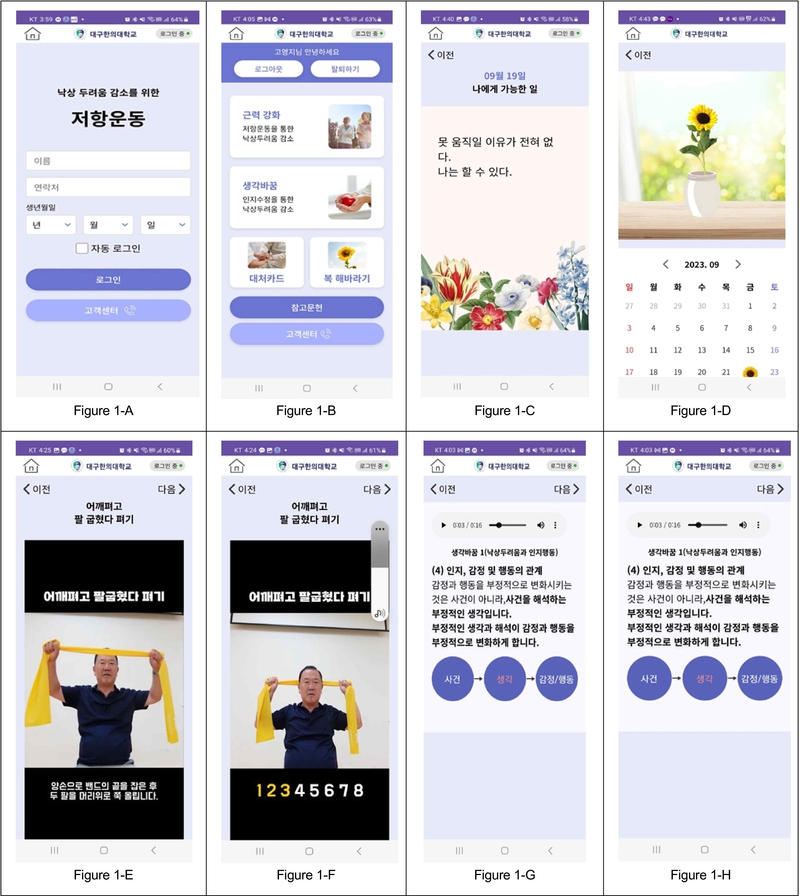
Through a collaboration with engineers, we designed the features and interface of the mobile application to visualize the content that would be included in a mobile-based exercise program. The mobile-based exercise application was developed from March to August 2023 over a 5-month course. After the mobile application developers implemented the prototype, several modifications were suggested by the researchers. We verified the organization and placement of the modified prototype screens, and that the application works as designed. The main screen of the application is demonstrated in Figure 1-A and B.
The multimedia cognitive behavioral education was loaded with written and voice formats into four mind health icons based on the contents created during the design phase. The education materials are available to participants at any time on the smartphones. A researcher has access to the master count to evaluate the opening of the corresponding screens of the participants, while individual participants do not have access to this data. The estimated time required to read or listen to all four “mind health” components is approximately seven minutes. Participants can also generate “coping card” by clicking on an icon. These cards will present the contents of the alternative thinking developed with input from a psychiatric nurse practitioner. The generated cards accumulate and are displayed on the screen, as shown in Figure 1-C.
Regarding the resistance training video, a video on how to use the Thera-band was loaded into the first icon in the exercise screen. Each exercise video was also loaded into each icon, and a video of all exercises combined was loaded into the last icon. The estimated duration of each exercise video is approximately two minutes, while the combined video lasts 19 minutes and 30 seconds. The participants were asked to click on the icon which indicates colors of the Thera-bands prior to exercise. The colors of the Thera-bands were composed of yellow, red, and green which indicate different intensities (Fahlman et al., 2011). Researchers can track the time participants spend watching the resistance training videos using the master log.
When participants achieve their exercise goal for that day, they can see a sunflower as positive feedback (Figure 1-D). The criterion that needs to be satisfied whether they reached their workout goals is the amount of time they watched the resistance training video. An individualized set alarm was established to maintain the resistance exercises. It was initially set twice a day (9 am and 4 pm) and its time and frequency will be revised according to interaction with participants. An additional alarm is set if the participants do not run the application. Alarm comments also emerge when they achieve the goal set. The researcher can update the frequency and comments of the alarm for the individualized resistance exercises at the master count.
RESULTS
1. Implementation and Evaluation of a Mobile-Based Exercise Program
Following the development of the mobile application, four experts downloaded the program onto their mobile phones and utilized it over a one-week period. Next, they provided feedback on the content and usability in a spreadsheet after development of the mobile-based exercise program. The team of experts included a psychiatric professor with more than 10 years of experience as a clinical psychologist, a rehabilitative medicine professor with more than 7 years of experience as a rehabilitation physician, a psychiatric nursing professor with about 5 years of experience of metacognition research, and a geriatric nursing professor with about 4 years of older adults’ frailty research experience.
They conducted a systematic review of the mobile application and suggested some points that required revisions. All experts perceived that the mobile application was useful and applicable in reducing FOF. The importance of eliciting core beliefs and expressing them on coping cards to remind older adults of their core beliefs was highlighted. They also believed that having a sunflower appear on the screen when a daily goal is completed was important and necessary for reinforcing positive behavior.
However, there were some comments for further improvement pertaining to the resistance training video and multimedia cognitive behavioral education. The mobile application was revised according to the experts’ comments through collaboration with engineers, but some comments could not be modified at this time. First, the font size on the phone screen could not be adjusted using fingers because this is a web-based application. Secondly, rewarding users with small gifts online was not feasible due to additional cost. Revision according to the experts’ comments is summarized in Table 1. Revision of the mobile application lasted for approximately 1 month. The screen of the resistance training and cognitive behavioral education is shown in Figure 1-E, F, G and H.
In addition, 10 older adults who had undergone hip fracture surgery and visited a teaching hospital evaluated the usability and satisfaction of the mobile application. A research assistant downloaded the application onto a hospital mobile phone and showed it to the participants, and assisted them to ensure they could use it thoroughly. Table 2 presents the participants’ survey results in terms of reliability, usability, effectiveness, accessibility, and satisfaction. The survey responses were rated on a 4-point Likert scale: 0 (Not at all), 1 (Slightly agree), 2 (Moderately agree), 3 (Strongly agree). The average effectiveness score was the highest at 2.60, while accessibility had the lowest at 2.10. Most older adults rated the application as reliable, easy to understand, helpful in reducing FOF, with a readable font and size, and satisfactory in its design.
2. Quality Assurance
An engineering expert and the first author conducted a systematic review to proactively detect bugs and defects when the final product was ready to be tested. Particularly, a final check was conducted to ensure that the targeted alarm times were working and that the contents were operating as intended.
DISCUSSION
Collaborative efforts involving a psychologist, exercise expert, and engineers were essential to developing a mobile-based exercise program. The contents for the cognitive behavioral education and exercise intervention were analyzed through comprehensive literature reviews. The resulting program integrated multimedia cognitive behavioral education, coping cards, resistance training videos, and positive feedback, with the development process spanning approximately five months. A key strength of this study is that the program provides accessible and effective interventions for reducing FOF and preventing falls. It enables older adults to exercise independently in their homes at any time. Moreover, periodic feedback and support may further enhance the program’s utility for this population. However, one challenge is that the application was not optimally configured for researchers; for instance, enabling font size adjustments would improve usability.
The use of smartphones by older adults for healthcare applications has been growing exponentially (Reyes et al., 2018). Particularly, the coronavirus disease 2019 has led to a significant increase in the use of mobile devices by older adults for accessing the Internet and information services (Liu et al., 2022). A mobile-based exercise program might be effective in reducing FOF provided that the difficulties that older adults may experience when using the application are addressed. Notably, a recent systematic review and meta-analysis (Lee et al., 2024) demonstrated that telehealth, exergaming, and mobile applications improved fall-related self-efficacy in older adults. This study specifically targets reducing FOF through a mobile-based exercise program for older adults after hip fracture surgery.
The mobile-based exercise program was based on cognitive behavioral principles to ensure the promotion and maintenance of the exercise program. CBT has been well-recognized in managing FOF in older adults (Chua et al., 2019; Liu et al., 2018; Whipple et al., 2018); however, it has been limited for older adults after hip fracture surgery and with non-face-to-face methods. Lim et al. (2023) found that an online 6-week CBT program was effective in terms of consequences of falling, concern about falling, stress, and social support for health for older adults. The online CBT was feasible, suggesting a high compliance and low attrition rate.
Conversely, a study (Whipple et al., 2018) revealed that unsupervised interventions or lack of ongoing support contact were non-efficacious in the management of FOF. Accordingly, this mobile application was developed to be used in conjunction with phone interactions for periodic checks and support. Goal setting for frequency and intensity of exercise, providing positive feedback, identifying unhelpful beliefs, and guiding alternative thinking are likely to be performed through an ongoing phone contact.
Evaluation of the mobile-based exercise program by experts and end users is a necessary process (Cody et al., 2020). Changes to enhance the quality of the application were employed through expert feedback, except for non-modifiable comments, such as adjusting the font size, which are considered as limitations of this study. In the end-user evaluation, the mobile application received the highest score for its effectiveness in helping to reduce FOF, while the lowest score was given for its accessibility, specifically in providing a readable font and size. In this study, the program is not suitable for older adults with a limited smartphone use, and the developed application is limited to Android; thus, users of other operating systems, such as that for iPhones (iOS) cannot use this application.
Despite these limitations, this study program was designed for frail older adults who have experienced hip fractures to perform resistance exercise, regardless of time or place. It incorporated cognitive behavioral education, goal setting, and positive feedback to maintain their motivation to exercise. The next step is to evaluate the long-term effect of the program for older adults after hip fracture surgery. Additionally, the involvement of significant others, such as spouses and family members, is crucial, as they can either exacerbate or alleviate FOF (Dolan & Pool, 2023). Their engagement in supporting older adults and encouraging continued use of the application is recommended. Finally, adequate education on resistance exercises using the application and the establishment of a trusting relationship should precede the implementation of the program to optimize its effectiveness.
CONCLUSION
This study developed an exercise program for older adults through mobile-based cognitive behavioral principles after hip fracture surgery. This program will likely contribute to FOF reduction in older adults after hip fracture surgery by replacing negative emotions with positive ones and improving physical strength and balance. An increase in the exercise program adherence is also expected. In future studies, the evaluation of the applicability and its efficacy for older adults is warranted.
Acknowledgments
This study was supported by the National Research Foundation of Korea (NRF), and funded by the Ministry of Science, ICT, and Future Planning (NRF-2020R1F1A104971111).
We would like to thank the individual who granted permission to use his photograph in this study.
REFERENCES
- Beck, J. S. (2017). Cognitive behavior therapy: basics and beyond (2nd ed.).Seoul: Hana Medical Publishing Co.
-
Chua, C. H. M., Jiang, Y., Lim, D. S., Wu, V. X., & Wang, W. (2019). Effectiveness of cognitive behaviour therapy-based multicomponent interventions on fear of falling among community-dwelling older adults: A systematic review and meta-analysis. Journal of Advanced Nursing, 75(12), 3299-3315.
[https://doi.org/10.1111/jan.14150]

-
Cody, J., Choi, J., & Martell, C. R. (2020). Developing an innovative tablet-based walking program to improve arthritis fatigue. Journal of Gerontological Nursing, 46(10), 13-18.
[https://doi.org/10.3928/00989134-20200909-03]

-
Delbaere, K., Close, J. C., Mikolaizak, A. S., Sachdev, P. S., Brodaty, H., & Lord, S. R. (2010). The falls efficacy scale international (FES-I): A comprehensive longitudinal validation study. Age and Ageing, 39(2), 210-216.
[https://doi.org/10.1093/ageing/afp225]

-
Dolan, H. R., & Pool, N. (2023). Overcoming waves of helplessness: the meaning of experiencing fear of falling. Geriatric Nursing, 52, 40-47.
[https://doi.org/10.1016/j.gerinurse.2023.05.003]

-
Fahlman, M. M., McNevin, N., Boardley, D., Morgan, A., & Topp, R. (2011). Effects of resistance training on functional ability in elderly individuals. American Journal of Health Promotion, 25(4), 237-243.
[https://doi.org/10.4278/ajhp.081125-QUAN-292]

-
Fragala, M. S., Cadore, E. L., Dorgo, S., Izquierdo, M., Kraemer, W. J., Peterson, M. D., & Ryan, E. (2019). Resistance training for older adults: Position statement from the national strength and conditioning association. The Journal of Strength & Conditioning Research, 33(8), 2019-2052.
[https://doi.org/10.1519/JSC.0000000000003230]

-
Ha, M., & Cho, G. (2023). Research of home-based exercise program development and effect analysis: prevention of sarcopenia in hemiplegic disorder. The Korean Journal of Rehabilitation Nursing, 24(2), 97-108.
[https://doi.org/10.7587/kjrehn.2021.97]

-
Jaatinen, R., Luukkaala, T., Helminen, H., Hongisto, M. T., Viitanen, M., & Nuotio, M. S. (2022). Prevalence and prognostic significance of depressive symptoms in a geriatric post-hip fracture assessment. Aging & Mental Health, 26(9), 1837-1844.
[https://doi.org/10.1080/13607863.2021.1998357]

-
Kendrick, D., Kumar, A., Carpenter, H., Zijlstra, G. R., Skelton, D. A., Cook, J. R., Stevens, Z., Belcher, CM., Haworth, D., Gawler, S. J., Gage, H., Masud, T., Bowling, A., Pearl, M., Morris, RW., Iliffe, S., & Delbaere, K. (2014). Exercise for reducing fear of falling in older people living in the community. Cochrane Database of Systematic Reviews, 11.
[https://doi.org/10.1002/14651858.CD009848.pub2]

- Kim, C. S., Park, I. H., Kim, M., Jang, S. H., Kim, Y. J., Park, M. H., et al. (2007). Effects of exercise using thera band on body compositions, blood pressure and physical fitness in the elderly women. Journal of Muscle and Joint Health, 14(2), 158-168.
- Kim, H. G., & Nam, H. K. (2011). The effect of thera band exercise on muscle flexibility, balance ability, muscle strength in elderly women. Research in Community and Public Health Nursing, 22(4), 451-457.
-
Ko, Y., Lee, J., & Baek, S. H. (2021). Discharge transition experienced by older Korean women after hip fracture surgery: A qualitative study. BMC Nursing, 20(1), 1-10.
[https://doi.org/10.1186/s12912-021-00637-9]

-
Ko, Y., Lee, J., Kim, S. Y., & Baek, S. H. (2019). Identification of factors related to functional decline of Korean older adults after hip fracture surgery: a cross-sectional study. Research in Gerontological Nursing, 12(6), 312-320.
[https://doi.org/10.3928/19404921-20190702-03]

-
Lam, D., & Gale, J. (2000). Cognitive behaviour therapy: Teaching a client the ABC model-the first step towards the process of change. Journal of Advanced Nursing, 31(2), 444-451.
[https://doi.org/10.1046/j.1365-2648.2000.01280.x]

-
Lee, K., Yi, J., & Lee, S. H. (2024). Effects of community-based fall prevention interventions for older adults using information and communication technology: A systematic review and meta-analysis, Health Informatics Journal, 30(2), 14604582241259324.
[https://doi.org/10.1177/14604582241259324]

-
Lee, S. J., Baek, S. H., & Ko, Y. (2023). A comparison of fear of falling in older adults with physical independence and those with hip fracture surgery. The Korean Journal of Rehabilitation Nursing, 26(1), 1-7.
[https://doi.org/10.7587/kjrehn.2023.1]

-
Lim, M. L., Tran, M., van Schooten, K. S., Radford, K. A., O'Dea, B., Baldwin, P., & Delbaere, K. (2023). A self-guided online cognitive behavioural therapy to reduce fear of falling in older people: A randomised controlled trial. International Journal of Behavioral Medicine, 30(3), 455-462.
[https://doi.org/10.1007/s12529-022-10105-6]

-
Liu, S., Wang, X. Q., Yang, B. X., Luo, D., Liu, Y., Fang, X. J., Ma, S., Kang, L., Huang, H-S., Lu, B., Zhao, J., Liu, Z., & Liu, Q. (2022). Electronic health literacy among older adults in the context of the COVID-19 pandemic: A mixed-methods study. Journal of Nursing Management, 30(6), 1949-1959.
[https://doi.org/10.1111/jonm.13664]

-
Liu, T., Ng, G. Y., Chung, R. C., & Ng, S. S. (2018). Cognitive behavioural therapy for fear of falling and balance among older people: A systematic review and meta-analysis. Age Ageing, 47(4), 520-527.
[https://doi.org/10.1093/ageing/afy010]

-
Lopez, P., Pinto, R. S., Radaelli, R., Rech, A., Grazioli, R., Izquierdo, M., & Lusa, E. (2018). Benefits of resistance training in physically frail elderly: A systematic review. Aging Clinical and Experimental Research, 30(8), 889-899.
[https://doi.org/10.1007/s40520-017-0863-z]

-
MacKay, S., Ebert, P., Harbidge, C., & Hogan, D. B. (2021). Fear of falling in older adults: A scoping review of recent literature. Canadian Geriatrics Journal, 24(4), 379-394.
[https://doi.org/10.5770/cgj.24.521]

-
Martinez-Arnau, F. M., Prieto-Contreras, L., & Pérez-Ros, P. (2021). Factors associated with fear of falling among frail older adults. Geriatric Nursing, 42(5), 1035-1041. https://doi.org.libproxy.dhu.ac.kr/10.1016/j.gerinurse.2021.06.007
[https://doi.org/10.1016/j.gerinurse.2021.06.007]

-
Montero-Odasso, M., van der Velde, N., Martin, F. C., Petrovic, M., Tan, M. P., Ryg, J., Aguilar-Navarro, S., Alexander, N. B., Becker, C., Blain, H., Bourke, R., Cameron, L. D., Camicioli, R., Clemson, L., Close, J., Delbaere, K., Duan, L., Duque, G., Dyer, S. M., ... Masud T. (2022). World guidelines for falls prevention and management for older adults: A global initiative. Age and Ageing, 51(9):afac205.
[https://doi.org/10.1093/ageing/afac205]

- Reyes, A., Qin, P., & Brown, C. A. (2018). A standardized review of smartphone applications to promote balance for older adults. Disability and Rehabilitation, 40(6), 690-696.
- Rovny, D. (2004). The scientific and clinical application of elastic resistance. Physical Therapy, 84(1), 109-110.
- Seels, B., & Richey, R. (1994). Instructional technology: The definition and domains of the field. Washington DC: Association for Educational Communication & Technology.
-
Trombetti, A., Reid, K. F., Hars, M., Herrmann, F. R., Pasha, E., Phillips, E. M., & Fielding, R. A. (2016) Age-associated declines in muscle mass, strength, power, and physical performance: impact on fear of falling and quality of life. Osteoporosis International, 27, 463-471.
[https://doi.org/10.1007/s00198-015-3236-5]

-
Wang, Q., Zhao, J., Huo, X., Wu, L., Yang, L., Li, J., & Wang, J.(2018). Effects of a home care mobile app on the outcomes of discharged patients with a stoma: A randomised controlled trial. Journal of Clinical Nursing, 27(19-20), 3592-3602.
[https://doi.org/10.1111/jocn.14515]

-
Whipple, M. O., Hamel, A. V., & Talley, K. M. (2018). Fear of falling among community-dwelling older adults: A scoping review to identify effective evidence-based interventions. Geriatric Nursing, 39(2), 170-177.
[https://doi.org/10.1016/j.gerinurse.2017.08.005]